Magnesium Supplementation and its Effects on Type 2 Diabetes Patients

Table Of Contents
What is Type 2 Diabetes?
Type 2 diabetes (T2D) is a long-lasting condition that can cause heart disease, stroke, kidney disease, blindness, and amputation. There are more than 400 million people who have diabetes worldwide and the prevalence is still increasing at an alarming rate. Several studies were conducted to improve the glycemic (or blood sugar) control indicators in T2D patients. They used different supplements, such as vitamin D, vitamin C, and dietary fibers, which have proven effective as potential diabetes risk modifiers. Furthermore, magnesium (Mg) supplements have been suggested to enhance the prevention and management of diabetes.
Can Oral Magnesium Supplementation Improve Insulin Sensitivity for Type 2 Diabetics?
Intracellular Mg levels are low in people with type 2 diabetes. Accompanied by increased intracellular free calcium (Ca), this may lead to insulin resistance. However, studies have shown that Mg supplementation can improve insulin sensitivity.
This study looked at the effects of including Mg supplementation on the typical diet of type 2 diabetes patients for three months.
The Study on Magnesium Supplementation for Type 2 Diabetic Patients
40 patients diagnosed recently (maximum of one year) to have T2D completed the study. They underwent a one-week dietary stabilization phase. They followed a prescribed diet plan to stabilize their serum glucose level. After which, they were stratified according to sex, age, fasting blood sugar (FBS), and Mg levels and then randomly and equally allocated into two groups. For three months, the intervention group was on 250 mg/day of elemental high-potency, highly absorbable Mg tablet. The other group did not receive any supplements throughout the intervention period.
Pertinent measurements and indicators were taken at the start of the study and after three months of intervention. Body Weight and height were measured to calculate body mass index.
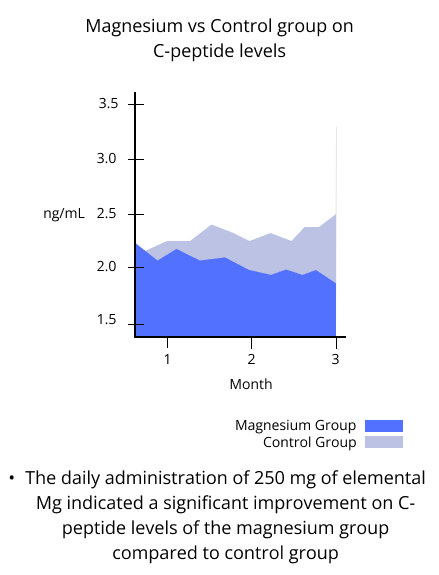
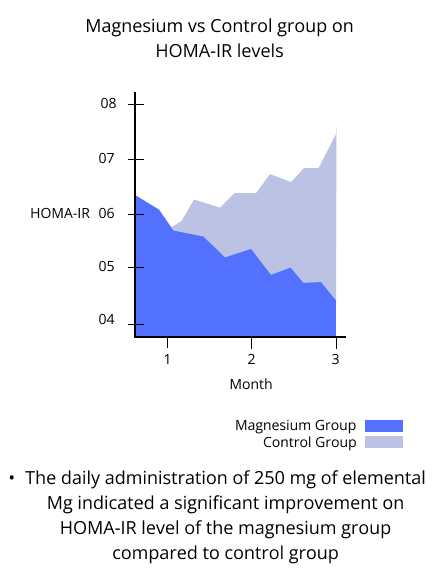
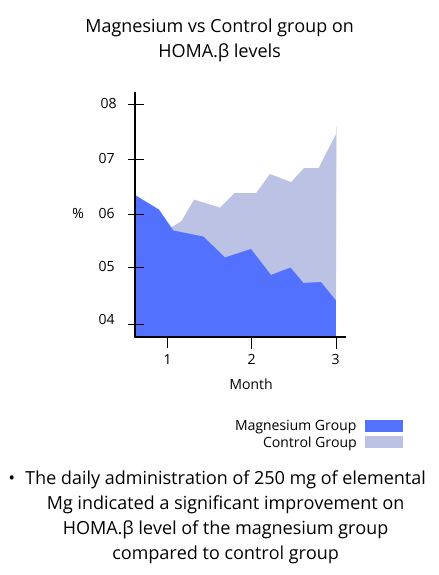
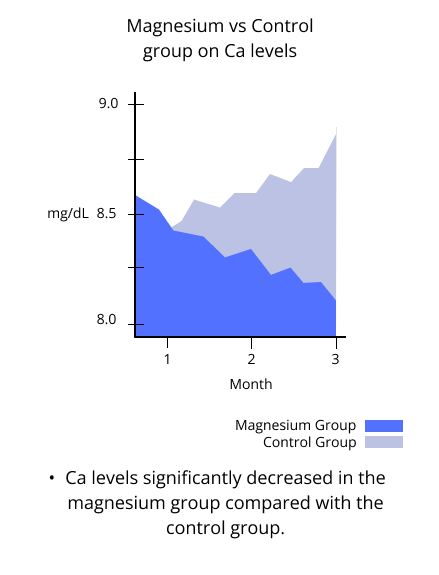
Blood samples were collected to analyze glucose and insulin indicators such as fasting blood sugar (or glucose), serum Ca, serum Mg, glycosylated hemoglobin (HbA1c), fasting C-peptide, and fasting insulin levels. Homeostatic model assessments of insulin resistance (HOMA-IR) and β-cell function (HOMA.β%) were computed to evaluate the relationship between glucose output and insulin secretion.
HbA1c refers to molecules of hemoglobin (a protein in the red blood cells) with glucose molecules attached, and is a reliable marker of insulin resistance. C-peptide is an amino acid that indicates how much insulin the body produces. HOMA-IR is a test that reflects how much insulin the body needs to control blood sugar levels, while HOMA.β% indicates how much insulin is secreted. High HOMA-IR and low HOMA-B were independently and consistently associated with increased diabetes risk.
The Results
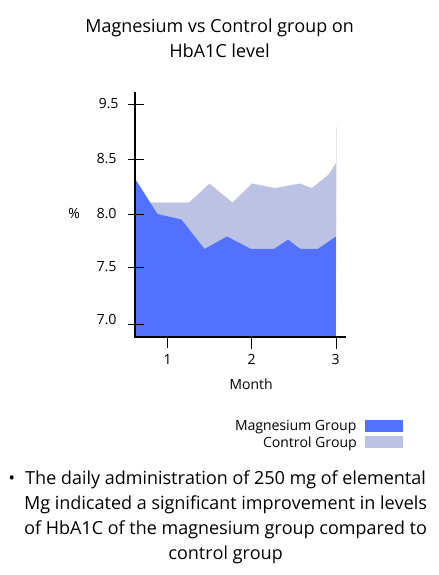
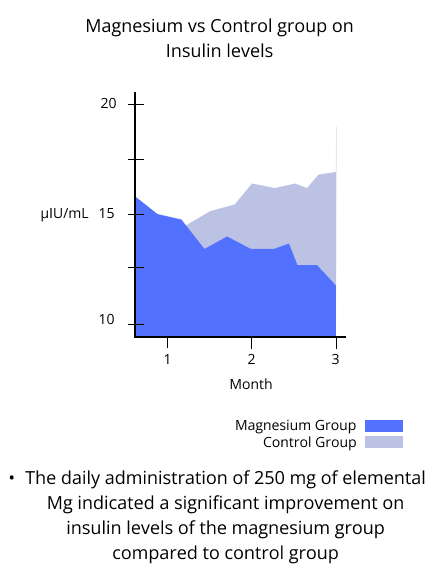
The daily administration of 250 mg of elemental Mg indicated a significant improvement in levels of HbA1C, insulin, C-peptide, HOMA.IR and HOMA.β% of the intervention group when compared with the control group after three months of intervention.
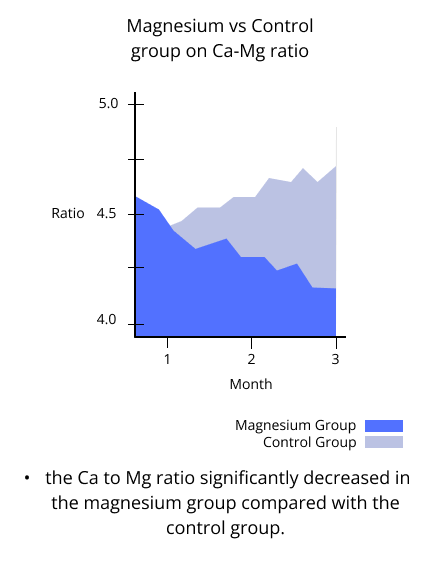
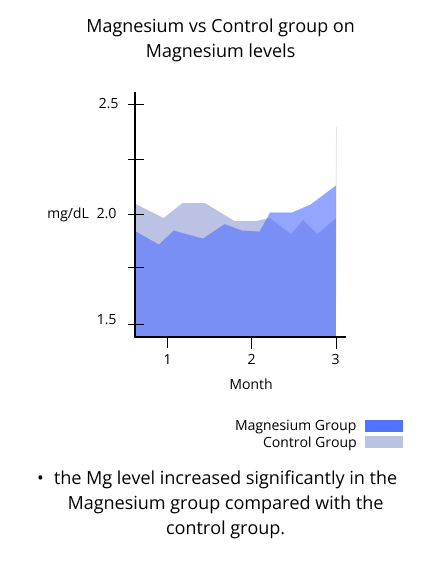
Ca levels and the Ca to Mg ratio also significantly decreased, while the Mg level increased significantly in the intervention group compared with the control group.
The Conclusion
This study looked at one of the disputed aspects of diabetes prevention and management. The results showed that oral magnesium supplementation significantly improved the levels of HbA1C, insulin, and C-peptide, HOMA IR, and HOMA β%, while decreasing blood sugar although insignificnatly. Additionally, magnesium supplements reduced insulin resistance and improved glycemic control indicators among T2D patients.
Reference
The Effects of Oral Magnesium Supplementation on Glycemic Response Among Type 2 Diabetes Patients
Related Posts
Quick Links
Legal Stuff