The Relationship Between Magnesium Sulfate, Cerebral Ischemia, and Subarachnoid Hemorrhage
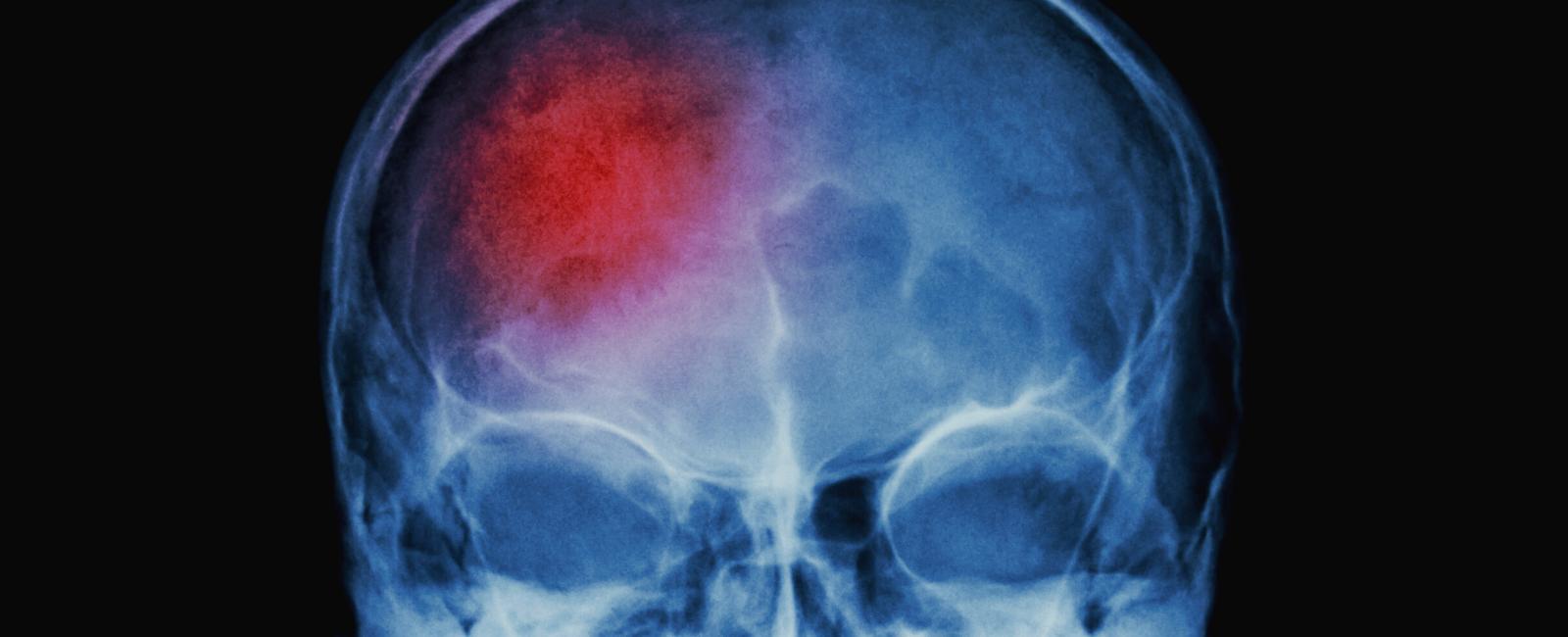
Table Of Contents
What is Cerebral Ischemia?
Cerebral ischemia is a brain stroke caused by a blocked artery that supplies blood to the brain. Subarachnoid hemorrhage is bleeding in the space surrounding the brain and is often due to a blood vessel that bursts and leaks, a condition called aneurysm.
What is Aneurysmal Subarachnoid Hemorrhage?
Aneurysmal subarachnoid hemorrhage (SAH) is a serious condition that often leads to death. Half of all patients die, and one out of every five survivors is left dependent on others. If a patient survives the initial hours after SAH and receives early treatment for the aneurysm, they are at risk for delayed cerebral ischemia (DCI). This situation occurs in about one-third of patients and usually happens between four and ten days after SAH.
Magnesium’s Potential for Brain Protection
Magnesium (Mg) therapy probably reduces the frequency of delayed cerebral ischemia (DCI) in subarachnoid hemorrhage (SAH) in a broad range of Mg concentrations. Still, uncertainty remains about the most desirable Mg concentration in the blood. If your Mg levels are too low or too high, it could have a harmful outcome.
Mg as a neuroprotective agent helps protect the brain from damage. A study found that half of those who had SAH did not have enough Mg in their blood. In another study, Mg sulfate given at a standard dose of 64 millimoles (mmol)/day reduced DCI incidence by 34%. At this dose, 85% of patients had Mg levels between 1.0 and 2.0 mmol/liter (l). Whether there is an ideal serum Mg concentration within this range is unclear.
We assessed the relationship between serum Mg concentrations achieved with Mg sulfate therapy and the incidence of DCI and poor outcome in patients with SAH.
The Study on Magnesium for Decreasing the Occurrence of Delayed Cerebral Ischemia
Included in this study were patients who had treatment for SAH. During their treatment, the placebo group had serum Mg concentrations below 1.10 mmol/l, while the Mg group, numbering 155, had at least 1.10 mmol/l. Those in the Mg group were put on 64 mmol/day Mg therapy within four days after SAH and continued medication for 20 days after SAH or until discharge from the hospital. All patients were treated according to a standardized protocol.
The Hijdra Score was used to assess the amount of blood in the brain on an initial computed tomography (CT) scan. This score was used to help predict how well a person will do after a SAH. The occurence of DCI was characterized by the presence of focal deficits (impaired functioning of the nerves, spinal cord, or brain) that gradually developed, decreased level of consciousness, or both, as confirmed by new lesions on CT. The clinical outcome (cure, degree of dis/ability, mortality) was assessed three months after SAH using the Rankin scale.
Differences in Mg concentrations between patients with and without DCI and with and without poor outcomes were calculated. Quartiles of last serum Mg concentrations before the start of DCI or Mg concentrations prior to the median day of DCI for patients without DCI were related to the incidence of DCI and poor outcome at three months using logistic regression.
The Results
Compared with the lowest quartile of serum Mg levels (1.10-1.28 mmol/l), the risk of DCI was lessened in each of the higher three quartiles. The odds ratio for poor outcome was 1.8 in the second quartile (Mg level of 1.29-1.40 mmol/l), 1.0 in the third quartile (Mg level of 1.41-1.62 mmol/l), and 4.9 in the highest quartile (Mg level of more than 1.62 mmol/l).
The Conclusion
Magnesium sulfate taken at 64 mmol/day results in a stable risk reduction of DCI over a wide range of achieved serum magnesium concentrations. Therefore, strict titration of the dosage does not seem necessary. However, concentrations of at least 1.28 mmol/l could decrease the effect on DCI, while concentrations of at least 1.62 mmol/l might result in poor clinical outcomes.
Reference
Related Posts



Quick Links
Legal Stuff